For decades, if not for a longer period, there have been attempts from within the church to make changes to the tradition of wearing religious uniforms by clergy. The above photograph is of Peter Owen-Jones who has some dress sense when trying to break down the barriers in communications with the faith followers. The Church of England Synod will decide in February 2014 if they are prepared to put power first or their parishioners.
It is a very serious matter. Dress can have disastrous consequences. Sadly, for example, there is evidence that there were increased suicide rates in an area where a Catholic nun, social worker wearing her habit was appointed for about four years.
SIGNIFICANCE OF RELIGIOUS UNIFORM WORN BY
MENTAL HEALTH PROFESSIONALS
|
To whom is religious uniform
significant
|
In what way is religious
uniform significant
|
|
Mentally ill person
|
Barrier to communication
It has already been established
by scientific research that no uniforms should be worn in mental health setting.
Thus one finds that doctors, nurses, social
workers and administrators in England have not worn any uniforms for at least
thirty years.
Uniforms are a barrier to
communications as in “us and them”. With impaired communication there is a much
decreased chance of effective diagnosis and treatment. The consequences of
wearing uniform defeat the purpose of employment.
Reminder of trauma
Men raped by clergy as children
experience flashbacks, panic attacks when reminders of trauma are presented
to them.
Diagnostic and Statistical
Manual of Mental Disorders TR IV lists diagnostic criteria for mental
illnesses. Under Post-traumatic disorder one is able to find that avoidance
is one of the groups of symptoms. Avoidance means avoiding situations and
people that act as reminders of the trauma. Talking about trauma is also a
reminder. Even thinking about appointments with professionals when such
traumatic events may be discussed can lead to anticipatory anxiety in
patients with Post-traumatic Stress Disorder. Some patients have sleepless
night(s) and even start vomiting when so anxious.
There is no point in
multiplying the barriers to communications with mentally ill people and
wearing of religious uniforms does just that for many.
Reminders of abuse by clergy include
religious uniforms. The result can be severe panic attacks experienced by
patients. Panic attacks are associated with higher mortality from myocardial
infarction too. Therefore, religious uniforms represent health and safety
risk in mental health setting that is preventable.
Uniform symbolic of uniformity
of values for the group wearing the same uniform
It is would be recognized by
most mentally ill people that uniform poses obligations on the wearer of
uniform to conduct themselves consistent with the values of the institution
it represents. This involves the sacrifice of individuality of the wearer.
The issues of trust arise out
of this situation. Person, who has given up their individuality and made considerable
efforts at it, is unlikely to uphold another person’s right to his/her
deviancy from norm (as in mental health issues) and especially so where the
degree of deviance from the norm can be considerable (healthy or unhealthy).
Health issues and stereotyping
There may be health issues that
patients would not disclose because of the fears of what religious person may
think about them, for example, sexual issues, family planning, abortions,
blood transfusions, epilepsy, mental
Illness causing behavioural
transgressions, hearing voices, feeling controlled by outside forces (as in
some cases of schizophrenia) and so on.
Reprisals
Disclosing history of abuse by
clergy to members of clergy has been very risky for victims. Now it is known
that canon law requirement has been to keep the history of abuse secret from
other people (including police) or risk excommunication.
In communities where clergy
have influenced even access to jobs fear of reprisals has been very real and
not evidence of paranoia. Unemployment creates depression, and exacerbates mental
illness. It can also lead to increased suicide risk.
Threats of reprisals against
the victims of abuse by clergy are some of the factors that prevented access
to state justice system. Mental health is damaged by chronic injustice and
this applies to victims, their families, and friends.
It has been argued by some
lawyers that aiding and abetting the crimes of child abuse happened at the
top of religious hierarchy through the cannon law defects as well as lack of
effective child protection measures following the disclosures of abuse. The
offenders were allowed to work not just within the same religious
organization but with children too while the risk of reoffending remained the
same. As crimes were not reported to police there would be no Criminal
Records Bureau check that would reveal anything.
Authority and power v right to
individuality
Healthy attitude is to accept
that each person is an individual. Religious uniforms represent authority and
power in mental health setting as determined by state that permits it.
Religious uniforms are misplaced in mental health setting as it actually
ignores patients’ need to be considered as an individual who may actually
hold very different beliefs and whose need at the time is his own health
foremost and not to be preoccupied with what the needs of the religious
person wearing religious uniform are. It is impossible to be faced with a
person wearing religious uniforms and not notice it unless one is blind or
has other rare perceptual disorders. This means that mentally ill person is
expected to adjust themselves to the expectations of the religious mental
health worker wearing the uniform irrespective of their desire, need or
ability to do so.
Equality issues through role modeling
Mental health workers are like
teachers in that they represent role models. It is unhealthy to act as a role
model for values that are against equality for women, those of different
ethnic groups, sexual orientation, different beliefs and so on. Religious
uniforms stand for patriarchal values and outdated values which are not in
keeping with the laws on equality.
Anxiety
Anxiety is common in many
mentally ill people and introducing more anxiety by wearing of religious
uniforms causes worry to patients and needless suffering which could be
prevented.
Putting patient in a situation
where he/she has to deal with making of formal objections to wearing of
religious uniforms also presents the task for mentally ill that they may not
be able to do. It is unreasonable to expect mentally ill, vulnerable people
to assert their rights and fight the system when even healthy professionals
are scapegoated and destroyed (see example of Dr Helen Bright) when they
attempt to do it.
Provocation and Violence
It can be said that religious
uniforms can represent provocation to some patients who already may have
problems with impulse control for various reasons such as high stress levels.
Some patients can be paranoid and grandiose too which in itself can lead to
poor impulse control and aggression towards those who are considered
irritants (like those wearing uniforms).
There are various cases of
murders of nuns and priests by mentally ill who had a mixture of paranoid and
religious delusions. The case of Mark Bechard is a well-known case and there
are many others. He killed at least two nuns in the same day and wounded
seriously more.
Mental handicap/Learning
Disability
It is recognised that there are
people who have severe cognitive handicaps, are very vulnerable and it can be
accepted that they may be totally unable to object themselves to the wearing
of religious uniforms or to even instruct anyone else to object on their
behalf to the wearing of religious uniforms by mental health workers. There
are sometimes large numbers of children with learning disabilities who
suffered abuse in the some religious institutions. Reminders of trauma may
not be verbalised but manifest themselves in behavioural deterioration which
would be difficult for professionals to manage or even understand in patients
with communications problems.
Suicides
a) Suicides can result from
untreated mental illness. When barriers to communications exist as they do in
human society and medical institutions for various reasons one finds
increased suicide rates. Men have higher suicide rates and there is social
expectation that men cannot be emotional, or sad. Gender inequality is
reinforced by most major religions and for both sexes in a different manner.
Sense of hopelessness may arise in patients when they see that mental health
institution they want and need to trust upholds values detrimental to their
health. Some religious people do not recognise manifestations of mental
illness but see it as possession by evil spirits which is offensive in itself
to mentally ill. We do know that medical regulator employs staff who have
such beliefs.
b) In Dr Bright’s case, she had no suicides
amongst her patients when working in a hospital where nun wearing her
religious uniform was employed as a social worker. However, there appeared to
be an increase in suicides following appointment of a nun wearing religious
uniform and after Dr Bright’s dismissal for raising the issue in the public domain.
Inefficient use of Taxes
It is now known that even as
much as 50% of UK population would at some point in their life experience
mental distress. In most case it would not come to the attention of
psychiatrists. The majority of those people would be working most of their
lives and paying taxes with which they would support the system that is not
supporting them at all times. When wearing of religious uniforms in mental
health is detrimental to patients it follows that using tax payers’ money for
salaries of people wearing them is inappropriate and against the interest of
the tax-payer too.
|
|
Doctors
|
Diagnosis and treatment
a) When there is no
communication or decreased or impaired communication between patient and
doctor wrong diagnosis and wrong treatment may result. Wearing of religious
uniforms impairs patient’ s communications with professional wearing it, and
even with those not wearing the religious uniform that become associated with
it in their minds. ”They are all the same” is what some say referring to all
the staff after a disappointment. This occurs in depressed patients and is
known as catastrophizing. The point here is that implications are wider than
one might think at first.
b) It is already established
that not wearing uniforms is associated with better compliance with
treatment, less absconding from wards, less self-harm, less violence from
patients. See paper by Roger C. Rinn.
Power
a) Some doctors can be unfair
and stigmatise mentally ill patients. This means that government policy of
leaving mentally ill at the mercy of local NHS Trust policy making is
misconceived when it comes to the wearing of religious uniforms by mental
health professionals. There is already discrimination against mentally ill
people and it is unlikely that all NHS Trust administrators would care about
mentally ill or that the majority of doctors would care about mentally ill as
much as about other patients assumed to be sane.
b) Medical profession is
self-regulated profession which means that it is possible to get rid of
dissident voices over a period of time through sham peer review process using
medical regulator such as the General Medical Council that has always been
religiously biased.
Raising the issue of religious
uniforms has been a dissident voice which puts patients first and not doctors
or other mental health professionals wearing religious uniforms.
British Medical Association is
conformist and it would support strike for doctors’ pensions for their
members but unlikely to take actions on human rights for patients and
especially not mentally ill.
Medical ethics is that patients
come first, but it does not happen in reality when religious uniforms are
worn by mental healthcare workers. However, it looks very nice in print that
patients come first.
Values and beliefs
Religious uniform may represent
the values that mental health professional holds important and prefer to hold
in isolation from other thoughts giving rise to cognitive dissonance such as
thoughts how bad it is for the patients and staff as well as the community
(public interest). Cognitive
dissonance plays a role in many value judgments, decisions and evaluations.
Becoming aware of how conflicting beliefs impact the decision-making process
is a great way to improve ability to make faster and more accurate choices.
This ideal awareness is not something that is likely to happen in medical
institutions dominated by men (General Medical Council in over 150 years
never had a woman President or Chief Executive) or where women are chosen for
their adherence to the same values and biases as men already there have. All
major religions are patriarchal and dear to some medical men for that very reason.
But not all medical men are the same.
|
|
Politicians
|
Votes
If it is accepted that
religious people vote and that getting those votes could make one believe
that by having religious bias at the expense of the mentally ill would lead
one to have more power if elected. The assumption here is that religious
people would prefer the rights of religious uniform to that of mentally ill
persons. There is no evidence that in the setting of having the knowledge
that uniforms (religious and non-religious) are harmful in mental health
setting the majority of religious people would be unreasonable and demand
special privileges to be given to those who wish to wear them. In fact, the
latest statistics show that the majority of UK citizens have secular views.
Power
Most religions are patriarchal
and that appeals to some politicians who may identify with such values. But
many would not if representative of the population and if asked.
Wilful Blindness
Some politicians may have been
well informed and knew that religious uniforms were, really, not such a good
idea in mental health setting but avoided dealing with the issues by creating
a good work wear policy because of cognitive dissonance and desire to
eliminate it by extolling the virtues of religion because of all the previous
personal investments made in religion.
|
|
Religious Institutions
|
Free Marketing
When religious uniforms are
seen in the setting where some good is done (health and social care)
religious institutions get free marketing because religious uniforms are
symbolic of religious institutions and their values. Doing the job of mental
health professional while wearing the religious uniform is perceived by
observer as the work of religious institution.
|
|
|
Power
Having the “right” to use
religious uniforms when other mental health professionals are not allowed to
do so places religious institutions in the positions of power and special privilege.
In fact, there is no such right in law.
It becomes impossible not to
consider the needs of the religious person in all interactions between
professionals and patients when religious uniforms are worn. Both
professionals and patients have at all time to consider what to say and what
not to say in fear of offending the religious and the institutions behind
them. Like in dysfunctional families one is walking on egg shells.
It is so very easy to offend
the religious.
|
|
|
Financial benefit
Religious uniforms are also
provocative and divisive.
Firstly, scientifically minded
professional is provoked to react to it. Similarly, person with sense of
justice could do the same.
Secondly, it is possible to
eliminate competition from scientifically orientated professionals by
claiming religious rights, establishing those rights as dominant rights and
thereafter benefiting financially when scientific competition is firstly
discredited and subsequently destroyed and eliminated from the workforce.
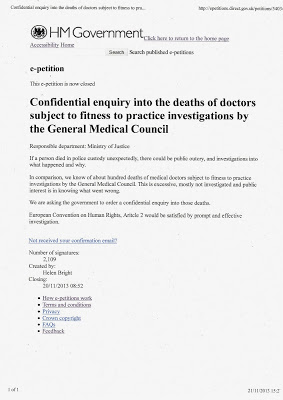
In the case of Dr Bright, she
was dismissed and erased from medical register while the nun was promoted and
remains registered with Social Care Council. The rights of mentally ill have
not been considered by anyone and how many died. This is breach of Article 9
of European Convention on Human Rights because religious rights are not
absolute rights as well as breach of Article 2.
|
|
General Public
|
Right to expression of
religious belief
While public recognize the
right to religious beliefs public expects politicians to put their health
first as well as the health of mentally ill. This would be in keeping with
European Convention on Human Rights Article 9, having the proper balance of
different rights.
|
|
Mental Health Institution
|
Image and values
In UK so far the social and
cultural background of institutional administrators determined preference for
the religious uniforms while disregarding the needs of the mentally ill. No
policies were created that eliminated the wearing of religious uniforms
anywhere in UK while it has been acknowledged that no uniforms are worn in
mental health setting normally.
Power
Where there is power there is
potential for abuse of that power. Low social status of mentally ill people
and low power of mentally ill enabled religious bias to dominate with fatal
consequences. Religious uniforms may be symbolic of values to which some administrators
aspire.
|
|
Justice system
|
High prevalence of abused
males
In a number of studies in penal
settings in Europe and elsewhere it has been established that there is high
prevalence of men who have suffered abuse as children including sexual. The
incidence is about 70%.
Considering the link of
traumatic experiences to that of offending one would have to consider the
impact of religious uniforms when visiting prisoners some of whom may have
suffered abuse by clergy.
There are men in UK prisons who
have killed clergy members following experiences of abuse by them.
|
|
Military
|
Murders by religious
psychiatrist wearing religious clothes
2009 USA Army base incident (Fort
Hood mass shooting by Dr Nidal Malik Hassan who killed 13 people and wounded
29) is a good example of failures to assess the risk to army personnel.
Here psychiatrist was seeing
army personnel some of whom would have post-traumatic stress disorder as the
result of the war in the country where predominant religion was Islam, the
same as that of the psychiatrist who dressed in ethnic clothes identifying
him as a Muslim. Patients with Post-traumatic stress disorder can be very irritable
and provocative and religious uniform is provocative itself. The combination
was fatal for many.
This incident happened 10 years
after Dr Bright warned about the wearing of religious uniforms in mental
health setting in UK which was published worldwide.
|
 Photograph from Daily Mail. Click on it to read the article
Photograph from Daily Mail. Click on it to read the article





 The e-petition Stop the badger cull is doing very well, indeed, and has secured more than enough votes to lead to a debate in the House of Commons.
The e-petition Stop the badger cull is doing very well, indeed, and has secured more than enough votes to lead to a debate in the House of Commons.
